The Effects of Earlier Medicaid Expansions: A Literature Review
The American Rescue Plan of 2021(ARP) temporarily increased the federal government contribution for Medicaid expansion to the 13 states that have not yet expanded Medicaid coverage to all low-income adults. Since the Affordable Care Act (ACA) expansion of Medicaid in 2014, there have been numerous studies that looked at its impact. These studies find first order effects including increased insurance coverage and improvements in health with no negative impact on state budgets. They also find second order, or indirect, effects such as gains in food security, housing security, financial wellbeing, and child support. These important effects have all come with little impact on state budgets as federal funding and decreases in state spending on uncompensated care, among other things, tend to cover the increased costs associated with expansion.
Background and Summary
Increasing health insurance coverage through Medicaid was a central goal of the ACA. Since its passage, a total of 36 states and D.C. have expanded Medicaid coverage to qualifying low-income adults and families, and Oklahoma has adopted but not yet implemented the Medicaid expansion (Kaiser Family Foundation, 2021a). The 13 states that have not adopted the Medicaid expansion are Alabama, Florida, Georgia, Kansas, Mississippi, Missouri, North Carolina, South Carolina, South Dakota, Tennessee, Texas, Wisconsin, and Wyoming.1 If all of these states expanded Medicaid, the Department of Health and Human Services estimates that about 4 million additional people would become eligible for Medicaid. They also estimate that the number of people eligible for Medicaid among uninsured Black adults in the 13 non-expansion states would increase almost fivefold, and it would increase sixfold among uninsured Hispanic adults (Branham et al., 2021).
The ARP includes a new financial incentive for states to expand their Medicaid programs. The provision increases states’ base Federal Medical Assistance Percentage (FMAP) by 5 percentage points for a period of two years for any non-expansion state that newly expands Medicaid coverage under the ACA. This increase is in addition to the ACA’s enhanced FMAP states receive for expanding coverage to low-income adults under the ACA, currently 90 percent. Assuming that all 13 non-expansion states begin their Medicaid expansion in FY2022, the federal government would contribute an estimated $14.4 billion over two years for the 5 percentage-point FMAP increase (Centers for Medicare & Medicaid Studies, 2021). A Kaiser Family Foundation (2021b) study found that for 12 of the non-expansion states the net fiscal impact would be positive following expansion.2 As discussed later in this paper, there is also evidence that expansion states have benefited from a net state-level savings from the ACA Medicaid expansion. Expansion states spend less on state uninsured programs (e.g. uncompensated care) and collect additional revenue from taxes that states levy on health care plans (Ward, 2020).
Expanding Medicaid coverage is also a form of economic stimulus that may be a useful policy tool to activate during an economic downturn that is accompanied by a major public health crisis. When the federal government increases its share of Medicaid costs (i.e. through increasing a state’s FMAP percentage), the extra federal spending allows states to use freed up state funds to meet other obligations. Indeed, Chodorow-Reich et al. (2012) found that additional federal Medicaid spending during the Great Recession increased state employment in sectors that are reliant on state funds (e.g. government, health, and education) and had even larger positive employment effects outside of these sectors. Hall et al. (2017) find that adults with disabilities were more likely to be employed in expansion states than in non-expansion states. A study of Medicaid expansion beneficiaries in Michigan found that they gained employment or were enrolled as students after a year with Medicaid (Tipirneni et al., 2020). These results are similar to Ku and Brantley’s (2021) estimate that the Medicaid expansion in the ARP will produce an additional 1 million jobs nationally.
A review of the literature focused on ACA Medicaid Expansions shows that increasing the federal share of Medicaid costs produces a variety of other effects beyond boosting employment in new Medicaid expansion states. In particular, our review suggests that, in addition to ACA Medicaid expansions improving health through greater access to health care, they also appear to promote health through raising incomes of low-income households (e.g. reduced hunger from less out-of- pocket health care costs) and information effects (e.g. reduced risky health behaviors from more exposure to doctors). They may also have beneficial non-health effects that operate through income effects, including greater financial security and less financially-motivated criminality. Below, we summarize key studies regarding the benefits associated with Medicaid expansion.
Literature Review
First Order Effects
By increasing insurance coverage, improving access to care and some health outcomes, the ACA appears to have met the stated goal of promoting health by covering a greater share of low-income Americans under Medicaid. Importantly, especially for states considering expanding Medicaid, studies show these improvements have been achieved without any additional pressure on state budgets.
- Coverage Effects
One of the primary goals of Medicaid expansion is to increase insurance coverage among low- income adults. The ACA Medicaid expansions have been successful in expanding coverage to low-income individuals. The Medicaid and CHIP Payment Access Commission (2020) found that, as of July 2020, Medicaid enrollment in expansion states has increased by 15.9 million, or 41.7 percent, from pre-expansion levels. Importantly, studies have found that increases in Medicaid coverage have not been offset by a decrease in private insurance (Frean et al., 2017). Medicaid expansion has also led to more continuous coverage. Goldman and Sommers (2020) find that Medicaid expansion has reduced disruption in coverage by 4.3 percentage points. This decrease in coverage disruption has been even more pronounced among perinatal women (Daw et al., 2020). Research also shows that children’s insurance coverage increased when their parents gained coverage, even though the children were eligible prior to expansion (Hudson and Moriya, 2017).
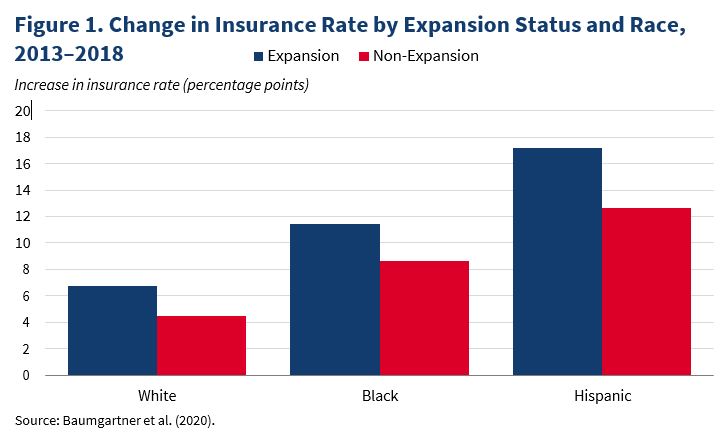
Expansions have also led to a narrowing of coverage disparities. Many uninsured low-income people of color became eligible for Medicaid in expansion states with the passage of the ACA, which raises the possibility that the reform mitigated racial health gaps. In a review of 65 studies, Guth et al. (2020) report that the balance of evidence shows that ACA Medicaid expansions helped narrow racial disparities in health insurance coverage, especially for Black and Latinx individuals. Between 2013 and 2018, there were larger increases in insurance rates for Blacks and Latinx than whites, with increases that were approximately 30-50 percent larger in expansion states compared to non-expansion states (figure 1) (Baumgartner et al., 2020).
- Access to care
Medicaid expansion has been associated with increases in access to, and affordability of, care. Studies have found that individuals in Medicaid expansion states are more likely to have a personal doctor and a regular source of care (Sommers et al., 2015; Simon et al., 2017). There has also been an increase in the treatment of chronic conditions, particularly through the increased use of prescription medications, including the treatment of substance use disorder (Gosh et al., 2018; Maclean and Saloner, 2019). Miller and Wherry (2019a) find that low-income individuals in expansion states were less likely to report that they could not afford needed medical care or that they delayed medical care due to cost. They also found a decrease in worrying about affording medical care. Similarly, McMorrow et al. (2017) find that low-income parents living in expansion states had reduced difficulty paying medical bills.
- Impact on health outcomes
Studies have also found that certain health outcomes improved under Medicaid expansion. In particular, Medicaid expansion has been associated with improved self-reported health, with earlier care, and with improved surgical outcomes (Sommers et al., 2017; Graves et al., 2020; Loehrer et al., 2018). The expansion was also associated with substantial improvements in mental health among low-income adults with chronic conditions (Winkleman and Chang, 2017).
ACA Medicaid expansions may have saved the lives of some newly insured low-income Americans because effective and timely health care treatment for an illness can prevent worsening health and death. Indeed, Borgschulte and Vogler (2020) found that ACA Medicaid expansions reduced all-cause mortality among non-elderly adults. This reduction which was largely driven by decreases in mortality in parts of the country with higher pre-expansion uninsured rates and by “amenable” causes of death that are plausibly preventable with access to adequate health care. Furthermore, a cost-benefit calculation performed by the authors suggests that the value of the lives saved may cover the entire net cost of the ACA Medicaid expansions. A more recent study finds that annual mortality in expansion states declined by 0.132 percentage points, or a 9.4 percent decrease relative to the sample mean (Miller et al., 2021).
- Impact on state budgets
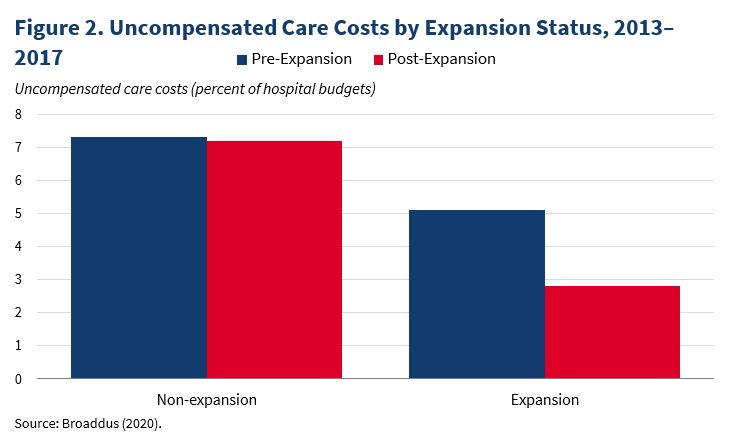
In addition to these health-related improvements among lower income individuals, ACA Medicaid expansions did not lead to increased state spending on Medicaid on net and has not reduced spending in other areas (Sommers and Gruber, 2017; Gruber and Sommers, 2020). This is likely due to reductions in state spending on mental health, corrections and uncompensated care costs for hospitals and clinics (Ward, 2020; see figure 2 for illustrative data drawn from Broaddus, 2020).
Second Order Effects
In addition to expanding health insurance coverage and the associated improvements in health outcomes, the literature has also documented a range of other beneficial secondary effects that may operate through two distinct channels. The first is a shift in consumer budget sets (i.e. an income effect). For instance, transitioning from being uninsured to insured—through a state Medicaid expansion—relaxes budget constraints of affected, low-income households, via reduced out‐of‐ pocket health care expenses. In turn, this increases the disposable income of those gaining health insurance coverage to meet other spending needs. Second, new health insurance coverage increases interactions with health professionals, so second order effects may operate through medical advice or educational materials that encourage healthy lifestyle choices (i.e. an information effect).
Taken together, the results below show that although the stated goals of the ACA Medicaid expansions did not consider many of the secondary outcomes subsequently studied in the literature, the benefits of expanded public health insurance clearly go well beyond health insurance coverage. Specifically, the literature has shown that ACA Medicaid expansions have resulted in gains in food security, housing security, financial wellbeing, and child support. They have also reduced crimes that can be borne out of economic despair and reduced risky health behaviors that can be explained by updates to health information sets that come with exposure to health professionals. And finally, studies have found that expanding Medicaid eligibility for pregnant mothers or young children generates a stream of beneficial effects on children’s later-life human capital and health outcomes.
To illustrate, we now discuss key studies within each of these topic areas.
- Food Security
Moellman (2020) found that ACA Medicaid expansions led to a reduction in the likelihood of food hardship, which was concentrated among households experiencing more serious food deprivation. Himmelstein (2019) also found that ACA Medicaid expansions reduced rates of very low food security.
- Housing Security
Allen et al. (2019) found that California’s early expansion of Medicaid through the ACA reduced evictions per capita, with the eviction reductions being concentrated among California counties with the highest pre-expansion uninsurance rates. Kuroki and Liu (2021) found that increases in the share of low-income people with health insurance induced by ACA Medicaid expansions increased homeownership rates among low-income people and housing prices of bottom-tier (i.e. lower priced) homes.
- Financial Wellbeing
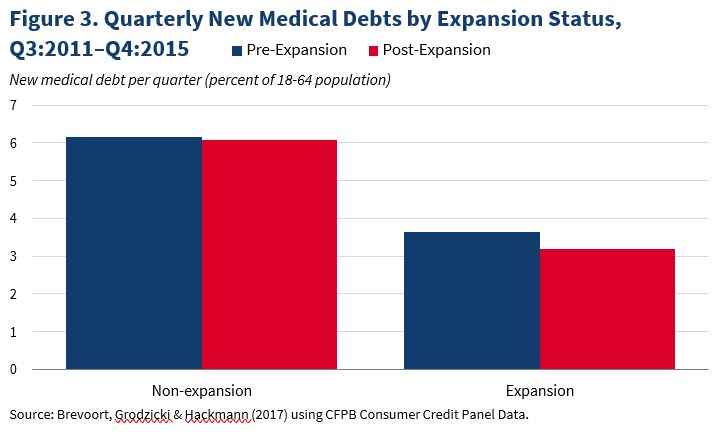
Hu et al. (2018) showed that ACA Medicaid expansions led to a decrease in levels of debt. Kuroki (2020) found that increases in the share of low-income people with health insurance brought upon by ACA Medicaid expansions reduced Chapter 7 bankruptcy rates, which is compelling since earning a low income is one of the requirements for filing a Chapter 7 bankruptcy. Brevoort et al. (2020) found that ACA Medicaid expansion led to a large aggregate reduction of medical debt valued at almost $6 billion, which, in turn, substantially reduced financial distress as measured by a reduction in the number of severe (credit/loan) delinquencies and improvement in credit scores. Brevoort et al. (2017) compared the accumulation of new medical debt per quarter before and after Medicaid expansion and found a decrease of over 12 percent in expansion states, compared to less than 1 percent in non-expansion states (figure 3).
- Child Support
Bullinger (2020) found that ACA Medicaid expansions increased past due and current child support distributed to custodial families. Taken together, the author estimates that, as a result of the ACA Medicaid expansions, these translate into an overall increase of $20 million in child support payments going to custodial families.
- Criminal Behavior
Vogler (2020) found that ACA Medicaid expansions led to a reduction in violent crime rates— which is largely explained by decreases in aggravated assaults—that translates into an annual social-cost savings of approximately $4 billion across the 31 states and District of Columbia that had expanded Medicaid.
- Health Behavior
Newly eligible Medicaid beneficiaries may receive advice from medical practitioners that lead them to adopt healthier behaviors. Consistent with this, studies have found that ACA Medicaid expansions were followed by dietary improvements (e.g. decreases in sugar content of beverage purchases) and reductions in risky health behaviors (e.g. decreases in cigarette consumption) (He et al., 2020; Cotti et al., 2019).
Effects of Childhood Exposure to Medicaid Expansions
The studies above focused on the shorter run outcomes of low-income Americans who gain health insurance coverage from ACA Medicaid expansions to adults. There is also evidence that children benefit from Medicaid expansions, both in utero and during childhood. Medicaid expansion generates positive long-run effects including better later-life health or human capital formation relative to those who were not covered by Medicaid. Given their long-term focus, these studies analyzed the effects of Medicaid expansions that occurred in the 1980s and 1990s.
Miller and Wherry (2019b) found that children whose mothers became eligible for Medicaid while they were in utero had improved later-life health outcomes (e.g. fewer hospital visits related to diabetes and obesity) as well as education outcomes (e.g. higher high school graduation rates). These improvements may have operated through improved access to or higher quality of prenatal care during pregnancy, which promote fetal health in ways that can have long-lasting beneficial effects.
Studies have also found that Medicaid eligibility expansions to children also produce positive long- run health and education effects.
Wherry et al. (2018) found that more years of Medicaid eligibility for Black children lead to fewer hospitalizations during adulthood. They estimate that the increased coverage led to a 7 to 15 percent decrease in hospitalizations at age 25. A back-of-the-envelope calculation suggests that the cost savings associated with this reduction in health care utilization among Black children at age 25 is equal to about 2–4 percent of the total cost of the Medicaid expansions to children of all races. Similarly, Wherry and Meyer (2016) found evidence of a decline in the disease-related mortality rate for Black children aged 15–18 after implementing non-ACA Medicaid expansions for children born after September 30, 1983. Boudreaux et al. (2016) also found evidence that early childhood exposure to Medicaid improved an index of health outcomes of individuals in their prime working years (25-54), which is shown to be partly driven by increases in the use of medical care for young children and reductions in family medical debt.
Improved childhood and adolescent health is often accompanied by improvements in human capital formation. Indeed, Cohodes et al. (2016) found that increases in childhood Medicaid eligibility reduced high school dropout rates and boosted college completion rates, along with evidence suggesting that better health during teen years was a driving mechanism of this result. Brown et al. (2020) also found that greater exposure to Medicaid during childhood led to higher college enrollment rates, lower fertility, and lower mortality rates in adulthood. The authors also found that more years of childhood Medicaid eligibility lowers benefits from the Earned Income Tax Credit program and increases federal tax payments, so that by age 28 the federal government regains 58 cents of each dollar it spends on children’s Medicaid coverage.
Conclusion
The benefits of Medicaid expansion far outweigh the costs. The FMAP increase included in the ARP incentivizes non-expansion states to expand Medicaid. The literature shows that Medicaid expansion improves insurance coverage and overall health. Medicaid expansion also improves
the financial outlook for recipients and provides long-term benefits for children that last generations.
1 Missouri is included because Governor Parson withdrew the State Plan Amendments related to expansion in May 2021.
2 Missouri is excluded from the study because the study was done before the State Plan Amendments were withdrawn.
References
Allen, H., E. Eliason, N. Zewde, and T. Gross. 2019. “Can Medicaid Expansion Prevent Housing Evictions?” Health Affairs, 38, no. 9: 1451–7. (Link)
Baumgartner, J., S. Collins, D. Radley, and S. Hayes. 2020. “How the Affordable Care Act Has Narrowed Racial and Ethnic Disparities in Access to Health Care.” The Commonwealth Fund Issue Brief. (Link)
Borgschulte, M. and J. Vogler. 2020. “Did the ACA Medicaid Expansion Save Lives?” Journal of Health Economics, 72: 102333. (Link)
Boudreaux, M., E. Golberstein, and D. McAlpine. 2016. “The Long-term Impacts of Medicaid Exposure in Early Childhood: Evidence from the Program’s Origin.” Journal of Health Economics, 45: 161–75. (Link)
Branham, D., C. Peters and B. Sommers. 2021. “Estimates of Uninsured Adults Newly Eligible for Medicaid If Remaining Non-Expansion States Expand.” Department of Health and Human Services Data Point. (Link)
Brevoort, K., D. Grodzicki, and M. Hackmann. 2017. “Medicaid and Financial Health.” NBER Working Paper 24002. Cambridge, MA: National Bureau of Economic Research. (Link)
Brevoort, K., D. Groadzicki, and M. Hackmann. 2020. “The Credit Consequences of Unpaid Medical Bills.” Journal of Public Economics, 187: 104203. (Link)
Broaddus, M. 2020. “Uncompensated Care Costs Well Down in ACA Medicaid Expansion States.” Center on Budget and Policy Priorities Blog. (Link)
Brown, D., A. Kowalski and I. Lurie. 2020. “Long-Term Impacts of Childhood Medicaid
Expansions on Outcomes in Adulthood.” Review of Economic Studies, 87, no. 2: 792– 821. (Link)
Bullinger, L.R. 2020. “Child Support and the Affordable Care Act’s Medicaid Expansions.”
Journal of Policy Analysis and Management, 40, no. 1: 42–77. (Link)
Centers for Medicare & Medicaid Studies. 2021. “All-State Medicaid & CHIP Call.” (Link) Chodorow-Reich, G., L. Feiveson, Z. Liscow and W.G. Woolston. 2012. “Does State Fiscal
Relief During Recessions Increase Employment? Evidence from the American Recovery and Reinvestment Act.” American Economic Journal: Economic Policy. 4, no 3: 118–45. (Link)
Cohodes, S., D. Grossman, S. Kleiner and M. Lovenheim. 2016. “The Effect of Child Health Insurance Access on Schooling: Evidence from Public Insurance Expansions.” Journal of Human Resources, 51, no. 3: 727–59. (Link)
Cotti, C., E. Nesson and N. Tefft. 2019. “Impacts of the ACA Medicaid Expansion on Health Behaviors: Evidence from Household Panel Data.” Health Economics, 28, no. 2: 219–44. (Link)
Cross-Call, J. 2020. “Medicaid Expansion Has Helped Narrow Racial Disparities in Health Coverage and Access to Care.” A report by the Center on Budget and Policy Priorities. (Link)
Daw, J., T. Winkelman, V. Dalton, K. Kozhimannil, and L. Admon. 2020. “Medicaid Expansion Improved Perinatal Insurance Continuity for Low-Income Women.” Health Affairs, 39, no. 9: 1531–39. (Link)
Frean, M., J. Gruber, and B. Sommers. 2017. “Premium Subsidies, the Mandate, and Medicaid
Expansion: Coverage Effects of the Affordable Care Act.” Journal of Health Economics, 53: 72–86. (Link)
Ghosh, A., K. Simon, and B. Sommers. 2018. “The Effect of Health Insurance on Prescription Drug Use Among Low-Income Adults: Evidence from Recent Medicaid Expansions.” Journal of Health Economics, 63: 64–80. (Link)
Goldman, A. and B. Sommers. 2020. “Among Low-Income Adults Enrolled in Medicaid, Churning Decreased After the Affordable Care Act.” Health Affairs, 39, no. 1: 85–93. (Link)
Graves, J., L. Hatfield, W. Blot, N. Keating and J.M. McWillians. 2020. “Medicaid Expansion Slowed Rates of Health Decline for Low-Income Adults in Southern States.” Health Affairs, 39, no. 1:67–76. (Link)
Gruber, J. and B. Sommers. 2020 “Fiscal Federalism and the Budget Impacts of the Affordable Care Act’s Medicaid Expansion.” NBER Working Paper 26862. Cambridge, MA: National Bureau of Economic Research. (Link)
Guth, M., S. Artiga, and O. Pham. 2020. “Effects of the ACA Medicaid Expansion on Racial Disparities in Health and Health Care.” An issue brief by the Kaiser Family Foundation. (Link)
Hall, J., A. Shartzer, N. Kurth and K. Thomas. 2017 “Effect of Medicaid Expansion on Workforce Participation for People With Disabilities.” American Journal of Public Health, 107, no. 2: 262–4. (Link)
He, X., R. Lopez, and R. Boehm. 2020. “Medicaid Expansion and Non‐alcoholic Beverage Choices by Low‐income Households.” Health Economics, 29, no. 11: 1327–42. (Link)
Himmelstein, G. 2019. “Effect of the Affordable Care Act’s Medicaid Expansions on Food Security, 2010–2016.” American Journal of Public Health, 109, no. 9: 1243–48. (Link)
House of Representatives. 2021. “H.R.1319 – American Rescue Plan Act of 2021.” (Link)
Hu, L., R. Kaestener, B. Mazumder, S. Miller and A. Wong. 2018. “The Effect of the Affordable Care Act Medicaid Expansions on Financial Wellbeing.” Journal of Public Economics, 163: 99–112. (Link)
Hudson, J and A. Moriya. 2017. “Medicaid Expansion for Adults Had Measurable ‘Welcome Mat’ Effects on Their Children.” Health Affairs, 36, no. 9: 1643–51. (Link)
Kaiser Family Foundation. 2021a. “Status of State Medicaid Expansion Decisions: Interactive Map.” (Link)
Kaiser Family Foundation. 2021b. “New Incentive for States to Adopt the ACA Medicaid Expansion: Implications for State Spending.” (Link)
Ku, L and E. Brantley. 2021. “The Economic and Employment Effects of Medicaid Expansion Under the American Rescue Plan.” The Commonwealth Fund Issue Brief (Link)
Kuroki, M. 2020. “The Effect of Health Insurance Coverage on Personal Bankruptcy: Evidence from the Medicaid Expansion.” Review of Economics of the Household, 19: 429–51. (Link)
Kuroki, M. and X. Liu. 2021. “The Effect of Health Insurance Coverage on Homeownership and Housing Prices: Evidence from the Medicaid Expansion.” Social Science Quarterly, 102, no. 2: 633–48. (Link)
Loehrer, A., D. Chang, J. Scott, M. Hutter, V. Patel, J. Lee and B. Sommers. 2018. “Association of the Affordable Care Act Medicaid Expansion with Access to and Quality of Care for Surgical Conditions.” JAMA Surgery, 153, no. 3. (Link)
Maclean, J.C. and B. Saloner. 2019. “The Effect of Public Insurance Expansions on Substance
Use Disorder Treatment: Evidence from the Affordable Care Act.” Journal of Policy Analysis and Management, 38, no. 2: 366–93. (Link)
McMorrow, S., J. Gates, S. Long and G. Kenney. 2017. “Medicaid Expansion Increased Coverage, Improved Affordability, and Reduced Psychological Distress for Low-Income Parents.” Health Affairs, 36, no. 5: 808–18. (Link)
Medicaid and CHIP Payment Access Commission. 2020. “Medicaid Enrollment Changes Following the ACA.” (Link)
Miller, S., N. Johnson, and L. Wherry. 2021. “Medicaid and Mortality: New Evidence from Linked Survey and Administrative Data.” NBER Working Paper 26081. Cambridge, MA: National Bureau of Economic Research. (Link)
Miller, S. and L. Wherry. 2019a. “Four Years Later: Insurance Coverage and Access to Care Continue to Diverge Between ACA Medicaid Expansion and Non-Expansion States.” AEA Papers and Proceedings, 109: 327–33. (Link)
Miller, S., and L. Wherry. 2019b. “The Long‐Term Effects of Early Life Medicaid Coverage.”
Journal of Human Resources, 54, no. 3: 785–824 (Link) MEDPAC “Medicaid enrollment changes following the ACA.” (Link)
Moellman, N. 2020. “Health care and Hunger: Effects of the ACA Medicaid Expansions on Food Insecurity in America.” Applied Economic Perspectives and Policy, 42, no. 2: 168–
86. (Link)
Simon, K., A. Soni, and J. Cawley. 2017. “The Impact of Health Insurance on Preventative Care and Health Behaviors: Evidence from the First Two Years of the ACA Medicaid
Expansion.” Journal of Policy Analysis and Management, 36, no. 2: 390–417. (Link) Sommers, B. and J. Gruber. 2017. “Federal Funding Insulated State Budgets from Increased Spending Related to Medicaid Expansion.” Health Affairs, 36, no. 5: 938–44. (Link)
Sommers, B., M. Gunja, and K. Finegold. 2015. “Changes in Self-reported Insurance Coverage, Access to Care, and Health Under the Affordable Care Act,” JAMA, 314, no. 4: 366–74. (Link)
Sommers, B., B. Maylone, R. Blendon, E.J. Orav, and A. Epstein. 2017. “Three-Year Impacts of the Affordable Care Act: Improved Medical Care and Health Among Low-Income Adults.” Health Affairs, 36, no. 6: 1119–28. (Link)
Tipirneni, R., J. Ayanian, M. Patel, E. Kieffer, M. Kirch, C. Bryant, J. Kullgren, S. Clark, S. Lee,
E. Solway, T. Chang, A. Haggins, J. Luster, E. Beathard, and S. Goold. 2020.
“Association of Medicaid Expansion With Enrollee Employment and Student Status in Michigan.” JAMA Network Open, 3, no. 1. (Link)
Vogler, J. 2020. “Access to Health care and Criminal Behavior: Evidence from the ACA Medicaid Expansions.” Journal of Policy Analysis and Management, 39, no. 4: 1166– 1213. (Link)
Ward, B. 2020. “The Impact of Medicaid Expansion on States’ Budgets.” Commonwealth Fund Issue Brief. (Link)
Wherry, L. and B. Meyer. 2016. “Saving Teens: Using a Policy Discontinuity to Estimate the
Effects of Medicaid Eligibility.” Journal of Human Resources, 51, no. 3: 556–88. (Link) Wherry, L., S. Miller, R. Kaestner, and B. Meyer. 2018. “Childhood Medicaid Coverage and
Later-Life Health Care Utilization.” Review of Economics and Statistics, 100, no. 2: 287–
302. (Link)
Winkleman, T and V. Chang. 2018. “Medicaid Expansion, Mental Health, and Access to Care
Among Childless Adults with and without Chronic Conditions.” Journal of General Internal Medicine, 33, no. 3: 376–83. (Link)

